Have you recently undergone a tummy tuck and noticed something unusual, like lumps, strange fluid, or slow healing? You might be dealing with a condition known as fat necrosis, a fairly common but often misunderstood side effect of abdominoplasty and similar surgical procedures like liposuction.
Understanding how fat necrosis affects the body is essential for anyone considering or recovering from a tummy tuck. The good news? Most cases can be managed effectively with early intervention and proper care. Let’s explore what it is, why it happens, and how you can treat or prevent it.

What is Necrosis After a Tummy Tuck?
Necrosis refers to the death of tissue in the body due to a lack of blood supply. In the context of tummy tuck surgery, this can affect skin or fat cells, particularly in areas where circulation has been disrupted. Fat necrosis is a type of necrosis where fatty tissue under the skin hardens or forms lumps. It may appear weeks after surgery and is typically benign, though it can be alarming to patients. Recognizing the signs early and understanding how and why necrosis occurs helps pave the way for proper treatment and smoother healing.
Types of Necrosis After a Tummy Tuck Procedure
Tissue necrosis after a tummy tuck can manifest in different forms, each with distinct causes, symptoms, and implications for recovery. Understanding the specific type of necrosis is critical for proper diagnosis and effective treatment. The two primary types encountered following abdominoplasty are fat necrosis and skin necrosis, which can be influenced by factors such as excess fat removal or poorly managed excess skin during surgery, each affecting the body in different ways.
Fat Necrosis
Fat necrosis occurs when fatty tissue beneath the skin dies due to disrupted blood supply, commonly caused by surgical trauma, ischemia, or post-operative complications. It typically appears as firm, rubbery lumps or nodules under the skin and may be accompanied by tenderness or slight discoloration. While fat necrosis can be visually and physically alarming, it is usually benign and not dangerous. Most cases resolve without intervention, although larger or symptomatic areas may require monitoring or minor treatment to ensure proper healing.
Skin Necrosis
Skin necrosis occurs when the skin tissue itself dies due to a significant loss of blood flow, often resulting from excessive tension on incisions, poor vascular supply, or surgical technique. This condition may appear as darkened, discolored patches in the necrotic area that can turn black and leathery in severe cases. Unlike fat necrosis, skin necrosis can pose a more serious threat to recovery and may require prompt medical intervention, including debridement or grafting, to remove dead tissue and promote proper healing.
Symptoms of Fat Necrosis After Tummy Tuck Surgery
Fat necrosis can present in various ways, and recognizing the signs of necrosis early can help avoid unnecessary worry or delayed treatment. While many symptoms are harmless and temporary, some may require medical attention. Here are the most common warning signs after tummy tuck surgery that patients may experience during their tummy tuck recovery.
Hard Lumps/Nodules
A rock-hard stomach after tummy tuck surgery is one of the most common signs of fat necrosis. The lumps often feel firm or rubbery beneath the skin and can vary in size. While they may seem concerning, they are usually harmless and tend to soften or shrink over time, sometimes disappearing completely on their own.
Changes in Skin Texture
The skin over areas of fat necrosis may feel uneven, thickened, or slightly dimpled. Some patients describe a “puckered” appearance where the fat has hardened beneath the surface. These changes are often temporary and may improve gradually as swelling subsides and healing progresses.
Skin Discoloration
Mild to moderate discoloration—such as red, purple, or yellowish tones—can occur around areas of fat necrosis. This can be due to bruising, inflammation, or tissue changes. While it may look alarming, it usually fades with time as the body reabsorbs damaged tissue and circulation normalizes.
Oily or Yellowish Fluid Leakage
Some patients notice a yellowish or oily discharge from the incision or surrounding tissue. This can result from fat breakdown and may indicate fat necrosis or fluid buildup. While not always a sign of infection, any unusual drainage should be reported to your surgeon to rule out complications and ensure proper healing.
Pain or Discomfort
Fat necrosis can cause mild to moderate discomfort, especially when pressure is applied to the affected area. The pain may feel dull or tender and is usually localized. Persistent or worsening pain should be evaluated, as it could also signal infection or other post-operative complications requiring medical attention.
Dimpling or Sagging
As the body absorbs necrotic fat tissue, the skin above it can lose support, resulting in dimpling or sagging. This cosmetic change is often subtle but may be noticeable, especially if larger areas are affected. In some cases, corrective procedures may be needed to restore a smoother contour.
Delayed Healing
Fat necrosis can slow down the normal healing process, especially if the affected area becomes inflamed or fluid-filled. You might notice scabs that don’t close, wounds that reopen, or incisions that take longer than expected to improve. Monitoring healing and reporting delays to your surgeon is crucial for preventing further issues.
SPECIALIST CARE YOU CAN TRUST
You can trust the entire staff to help make your visit as comfortable and safe as possible!
What Causes Necrosis After a Tummy Tuck
Fat necrosis and other tissue damage after a tummy tuck can result from several different factors. Some are related to the body’s healing process, while others may stem from surgical techniques or lifestyle habits. Understanding these causes is key to both preventing and properly treating complications when they arise.
Ischemia
Ischemia refers to restricted blood flow, which can deprive tissues of oxygen and nutrients needed for healing. During a tummy tuck, if the blood supply to certain areas is compromised—often due to tension or surgical disruption—tissue death can occur, increasing the risk of necrosis, particularly in the lower abdominal flap.
Infection
Post-surgical infections can interfere with the healing process and contribute to tissue breakdown. When bacteria spread to the surgical site, they can trigger inflammation and weaken nearby fat and skin, making the area more vulnerable to necrosis. Early treatment is essential to prevent more serious complications.
Trauma
Accidental trauma to the surgical site—such as bumping, falling, or applying too much pressure—can damage healing tissues and compromise blood supply. Even something as simple as improper compression garment use may cause localized injury, leading to fat necrosis or delayed healing in the affected area.
Smoking
Smoking significantly reduces oxygen levels in the blood and impairs circulation, both of which are crucial for proper healing after any cosmetic surgery. Nicotine also narrows blood vessels, increasing the risk of ischemia and tissue damage. Patients who smoke are at much higher risk for developing fat necrosis and other complications post-tummy tuck.
Underlying Medical Conditions
Conditions like diabetes, autoimmune disorders, or vascular disease can impair blood flow and the body’s natural healing response. These issues increase the risk of complications such as necrosis. Patients with chronic health conditions should undergo thorough pre-operative assessments and follow all medical advice to support proper healing.
Improper Technique
Surgical experience and precision play a major role in reducing complications. If too much tissue is removed or excessive tension is placed on incisions, it can limit blood flow and increase the chance of necrosis. Choosing a skilled, board-certified surgeon is crucial for optimal technique and safer results.
Post-Operative Care
Neglecting proper post-surgical care can lead to infection, poor healing, and fat necrosis. Skipping follow-up appointments, wearing garments incorrectly, or ignoring wound care instructions may all contribute to complications. Closely following your surgeon’s recovery plan gives your body the best chance to heal safely and successfully.
Diagnosis Methods for Post-Tummy Tuck Fat Necrosis
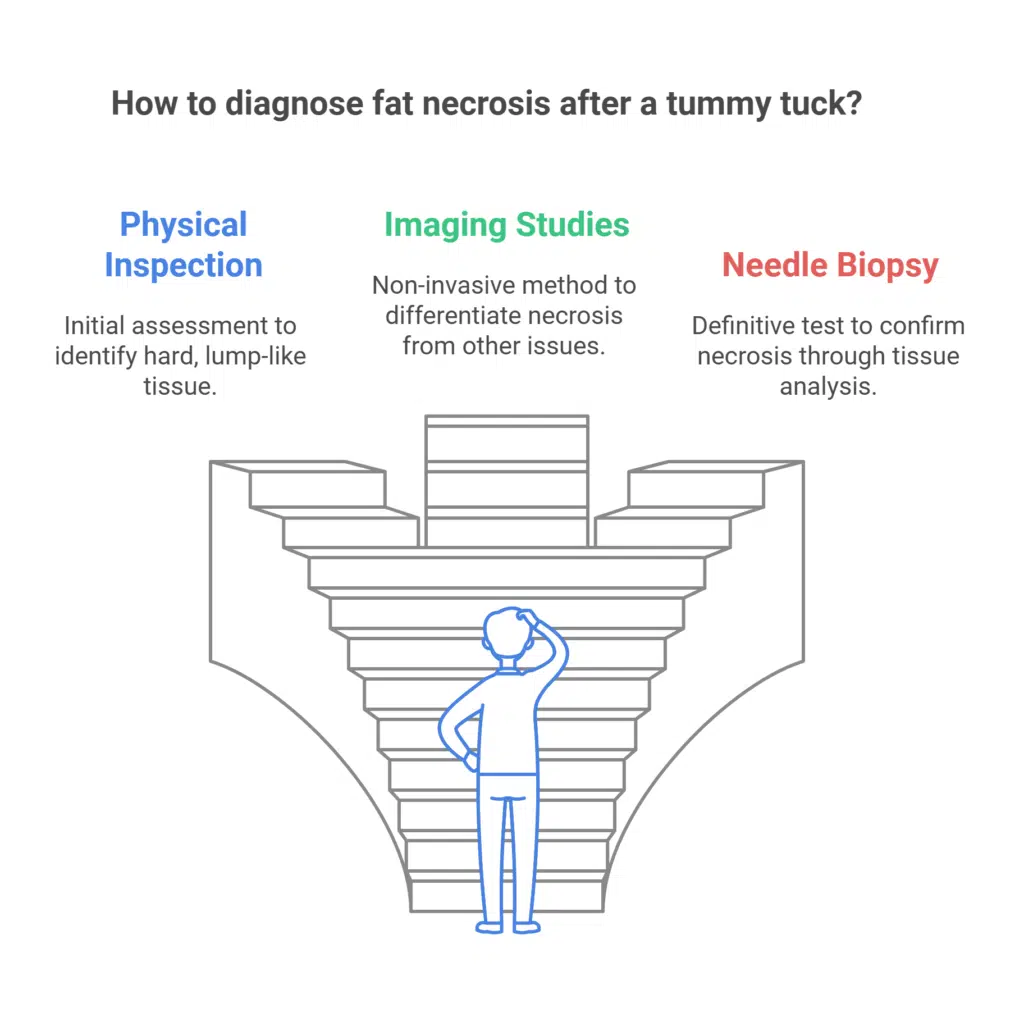
Diagnosing abdominoplasty necrosis calls for multiple methods. At first, a physical inspection is critical. As we have noted, fat necrosis sometimes feels to be a hard, lump-like section of the fatty tissue. This rigidity is not like the milder sensation of typical post-operative edema or scar tissue. A common feature of necrosis is that a cyst-like structure may also be revealed when the affected area is palpated.
Imaging studies can offer more proof if physical findings point to fat necrosis. A non-invasive technique called ultrasonic imaging distinguishes between fat necrosis and other possible consequences, including symptoms of infection or fluid collection.
Should imaging be unsatisfactory, a needle biopsy procedure can be carried out. Tissue from the questionable location is taken out during this operation using a tiny needle. The sample is then examined under a microscope to guarantee that necrosis exists.
Differentiating fat necrosis from other issues is vital to make sure patients get the right advice and treatment for their post-operative recovery.
Treatments for Fat Necrosis After Tummy Tuck
Most cases of fat necrosis resolve on their own with time and close monitoring. However, if symptoms persist or become uncomfortable, there are several treatment options available. The goal is to reduce inflammation, relieve discomfort, and restore the smooth appearance of the abdominal area.
Conservative Treatments
- Massage and Compression Garments: Help reduce swelling, improve circulation, and assist the body in breaking down necrotic fat naturally.
- Warm Compresses: Promote blood flow to the affected area, aiding the healing process and reducing discomfort.
- Ultrasound Therapy: Sometimes used to help break up firm fatty nodules and encourage absorption by the body.
- Aspiration: If fluid builds up, a needle may be used to drain it and reduce pressure.
- Anti-Inflammatory Medications: Prescribed to relieve pain and minimize swelling around affected tissue.
Surgical Options and Advanced Treatments
- Debridement: Surgical removal of necrotic or non-viable tissue to prevent further spread and aid in healing.
- Fat Grafting: After debridement, surgeons may fill the area with healthy fat to improve contour and minimize scarring.
In all cases, consistent follow-up care is essential to monitor recovery, ensure effective treatment, and prevent recurrence. Your plastic surgeon will tailor a plan based on the extent of necrosis, your overall health, and your aesthetic goals.
Before and After Photos


* Each patient is unique and individual results may vary.
Possible Complications of Necrosis Post Abdominoplasty
While fat necrosis is usually manageable, it can occasionally lead to further complications—especially if left untreated. Some issues may be mild and temporary, while others could require additional cosmetic procedures or medical care. Being aware of potential complications helps patients take action early and improve their recovery outcomes.
Mild or Short-Term Complications
- Prolonged Swelling: Swelling in the affected area may linger longer than usual.
- Skin Irregularities: Lumps, dimpling, or firmness can affect the appearance of the abdomen.
- Temporary Pain or Sensitivity: Discomfort may persist for weeks as the tissue softens and heals.
- Delayed Wound Healing: Necrosis can slow the closing of incisions or create small wound openings.
- Gradual Reabsorption: The body may naturally absorb necrotic fat tissue over time, leading to slow but steady improvement.
- Persistent Lumps or Fatty Deposits: Some lumps after tummy tuck may remain for extended periods, though they are often harmless and stable.
More Serious or Long-Term Complications
- Infection: If necrotic tissue becomes infected, it may lead to cellulitis or abscesses.
- Scarring or Skin Loss: Severe cases can result in visible scars or the loss of skin tissue.
- Tissue Recession or Deformity: Damage to fat and skin can cause indentations or irregular contours.
- Need for Revision Surgery: Persistent or severe cases may require surgical correction, such as fat grafting or scar revision.
- Seroma: Fluid accumulation beneath the skin may develop and require drainage if it doesn’t resolve naturally.
- Deep Vein Thrombosis (DVT): Though rare, limited mobility during recovery can increase the risk of blood clots, which require immediate medical attention.
How to Prevent Fat Necrosis After Tummy Tuck
While not all cases of fat necrosis are preventable, there are several steps you can take to significantly lower your risk. Prevention begins with choosing a qualified surgeon and continues through attentive aftercare. Following your provider’s instructions closely gives your body the best chance to heal cleanly and avoid complications.
Follow Strict Wound Care
Proper wound care is essential for preventing fat necrosis and other complications. Follow your surgeon’s instructions precisely—keep the incision area clean, dry, and covered as recommended. Avoid applying any products that weren’t approved, and report signs of infection, like redness or unusual discharge, as soon as they appear.
Wear Compression Garments
Compression garments support healing by minimizing swelling and encouraging healthy blood flow to the surgical site. They also help maintain contour and reduce the risk of fluid buildup or skin irregularities. Be sure to wear them as directed—too tight or too loose can lead to complications.
Hydration and Diet
Staying hydrated and eating a balanced diet rich in vitamins, protein, and antioxidants gives your body the tools it needs to heal efficiently. Proper nutrition supports tissue repair, reduces inflammation, and boosts your immune response—key factors in preventing complications like necrosis after tummy tuck surgery.
Avoid Excessive Pressure
Applying too much pressure to healing tissue can disrupt blood flow and increase the risk of fat necrosis. Avoid tight clothing, pressing on the abdomen, or sleeping on your stomach. Always follow your surgeon’s recommendations for safe movement and positioning during the early recovery period.
Restrict your Movements
Limiting physical activity after surgery helps your body focus on healing and prevents strain on the abdominal area. Avoid lifting, bending, or exercising until cleared by your surgeon. Overexertion too soon can interfere with circulation, slow healing, and increase the risk of post-op complications like fat necrosis.
Choose an Experienced Plastic Surgeon
Choosing an experienced plastic surgeon is key to minimizing the risk of fat necrosis and other complications after a tummy tuck. Expertise in surgical technique, careful patient evaluation, and proper post-operative planning all play a vital role in ensuring the best possible outcome and long-term satisfaction.
At Aesthetic Surgical Images in Omaha, NE, our team of board-certified plastic surgeons offers a combined wealth of experience and collaborative insight. Our surgeons are ACLS certified and deeply committed to patient safety and care. We take pride in delivering tailored treatment plans to meet your needs and support your recovery journey every step of the way. Call us today at 402-390-0100 or visit our contact page to schedule your consultation.